Visceral fat—the deeper belly fat that accumulates around the organs of the abdominal cavity, is linked to many health disorders that include heart disease, type 2 diabetes, high blood pressure (hypertension, and dementia.
With the evidence mounting on the associations between obesity, heart disease (CVD), and type 2 diabetes (T2D), to an increased risk for Alzheimer’s disease, an increased awareness of these associations and how it is all connected, now appears regularly in many popular news feeds.
One such association I will elaborate on here is how visceral fat and it’s association with chronic inflammation is a risk for brain shrinkage as you age. Yes, you read that correctly—brain shrinkage!

Brain and Hippocampal Atrophy
Brain shrinkage is one of the primary factors linked to cognitive decline in the aging process, and the progression from normal cognition to mild cognitive impairment (MCI), and the eventual diagnosis of late-onset Alzheimer’s disease (LOAD). A greater loss of brain volume is a biomarker that signifies that you are greater greater risk for LOAD.
Structural magnetic resonance imaging (MRI) has emerged as a pivotal biomarker assessment in evaluating brain and hippocampal volume and volumetric changes over time.(2) MRI evaluations of hippocampal volume and volumes of other brain regions are considered as a reliable index of Alzheimer’s neuropathology.(2,3)
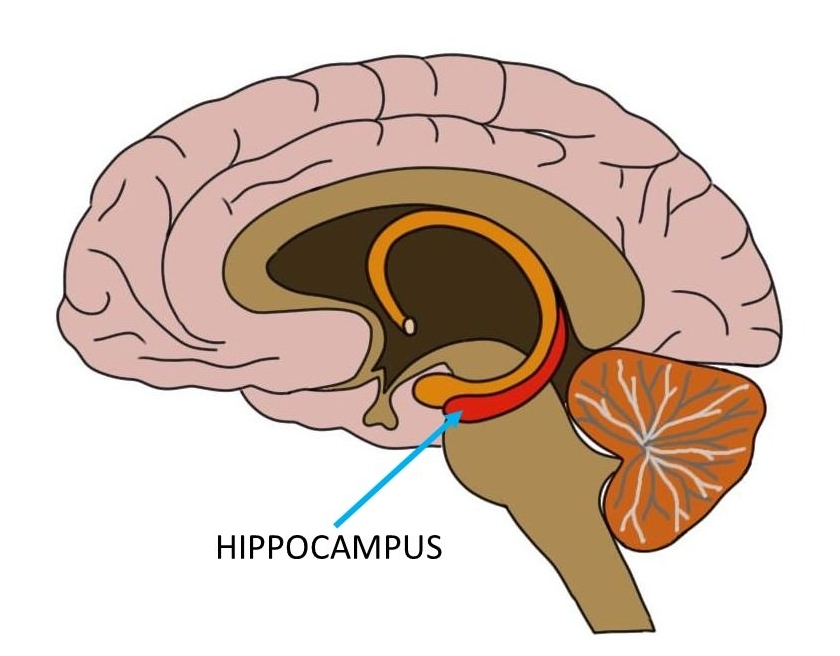
The hippocampus and associated structures of the hippocampal formation that includes the hippocampus proper (e.g., cornu ammonis), dentate gyrus, and the subiculum, are the hub of memory and learning mechanisms.
The loss of volume and changes in the shape of the hippocampus are seen in the earliest stage of LOAD—the pre-clinical stage which is sans any observable signs or symptoms associated with cognitive decline.
In my book, The Diabetic Brain in Alzheimer’s Disease, I emphasize how critical it is to take control over the risk factors at midlife, or earlier, that put you and your brain at risk for cognitive decline and dementia as you age. The Alzheimer’s disease process spans at least twenty to thirty years before an eventual diagnosis which highlights the importance of early assessment and intervention approaches.
Back to brain shrinkage…the findings of a recent study (1/2019), detailed the associations between increased visceral fat and obesity to brain shrinkage (atrophy). It did not report on hippocampal volume changes. White and gray brain matter and volumes in the various regions of the brain were tracked via MRI.
9,652 people were included in the study analysis and the average age of the people was 55. Body mass index (BMI), a weight to hip ratio (WHR), and overall body fat was evaluated. “19 percent of the study participants were determined to be obese.”
A higher BMI and WHR correlated to “the lowest average gray matter brain volume.”
This is not the first study to arrive at such a conclusion.
“The Northern Manhattan Study”, a research study of stroke and stroke risk factors in the Northern Manhattan community, participants with an average age of 64 and a BMI greater than 30, “exhibited a smaller cortical thickness” over participants with a BMI under 25. The study researchers concluded that “Adiposity (excess fat, obesity) in early-old age is related to reduced global gray matter later in life…”
Other studies have shown that visceral fat and chronic inflammation as key mediators of brain shrinkage.(5,6)
As illustrated in The Diabetic Brain in Alzheimer’s Disease, belly fat is a source of pro-inflammatory molecules termed cytokines.
Cytokines and other markers of inflammation are associated with reductions in total brain volume, and to the onset of Alzheimer’s and dementia later in life. See illustration from the book below.
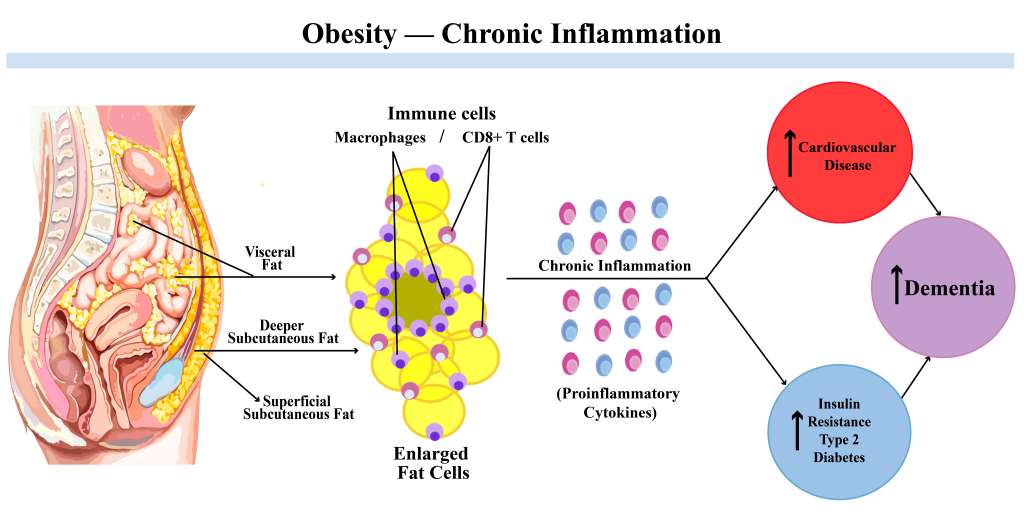
Illustration from The Diabetic Brain in Alzheimer’s Disease
What about the hippocampus? Several studies have shown that visceral fat (deeper belly fat) is associated with hippocampal atrophy too.
A 2011 study demonstrated the association between a higher body mass index (BMI) and reductions in hippocampal volume.(7)
Another 2011 study that included 184 healthy Chinese volunteers recruited from the “Singapore-Longitudinal Aging Brain Study” without cognitive impairment, higher deposition of visceral adipose tissue “was associated with lower hippocampal volume.” The study criteria excluded participants with a history of diabetes or “significant events (i.e., myocardial infarction, stroke, or peripheral vascular disease).
The “Australian PATH Through Life Study” that included 420 unimpaired community dwelling participants 60 to 64 years of age and tracked over eight years, revealed that being overweight or obese (higher BMI) correlated to lower hippocampal volume.
I could go on, but no need to cite study after study that has shown a distinct correlation between being overweight or obese, and higher visceral fat deposition, to a lower brain and hippocampal volumes.
Skinny fat and Sarcopenia
Now, there is another body type that outwardly appears to be lean, but is metabolically obese and normal weight (MONW)—the skinny fat body type. These skinny fat types will generally not be on the radar of many physicians as they fall into a normal body mass index (BMI) classification that is based on the ratio of weight to height.
Nonetheless, like many overweight or obese types that have excess belly fat, skinny fat individuals are at higher risk for metabolic syndrome, insulin resistance and type 2 diabetes, and cardiovascular disease (cardiometabolic disease).
Apart from the increase in body fat associated with aging, the loss of lean body mass in aging (sarcopenia) incurs risks linked to cognitive decline, dementia, and brain atrophy.
The term sarcopenia denotes a loss of muscle mass and strength in an individual, and it is a condition that is not uncommon in aging individuals.
Sarcopenia may begin as early as the fourth decade of life, and up to 50% of lean body mass is lost by the eight decade of life.(9) Malnutrition, smoking, hormone imbalances, mitochondrial dysfunction, chronic inflammation, genetic risk factors, and lack of exercise are predisposing factors for sarcopenia, as are age-related diseases and many other chronic health disorders.
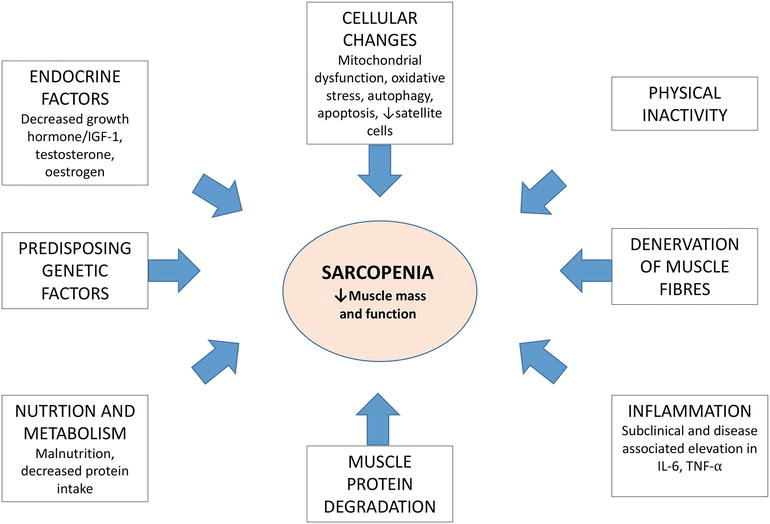
Attribution: “Epidemiology of Sarcopenia and Frailty”—CC BY 3.0
http://dx.doi.org/10.5772/intechopen.69771
Just as metabolically obese normal weight individuals display a reduced lean muscle mass and increased body fat mass, sarcopenia is typified by the same disproportionate alterations in the fat to lean muscle mass ratio and is termed sarcopenic obesity.
The results of a study (2018) that included 353 participants with an average age of 69 years, determined that sarcopenic obesity (loss of muscle mass and increased fat mass/obesity) was associated with “the lowest performance on global cognition, followed by sarcopenia alone and then obesity alone.” This first of its kind study concluded that “Sarcopenia alone and in combination with sarcopenic obesity can be used in clinical practice as indicators of probable cognitive impairment.”(10)
The takeaway for the points on sarcopenia and sarcopenic obesity? If you are an aging person and not exercising, your couch potato lifestyle may put you into the classification of a skinny fat individual with the same cardiometabolic disease risk factors associated with insulin resistance in prediabetes/type 2 diabetes.
Not surprisingly, diabetes is linked to a shrinking brain. In “The Hisayama Study” that included 1,238 community-dwelling Japanese, the authors concluded that “that a longer duration of diabetes and a midlife onset of diabetes are significant risk factors for hippocampal atrophy, a main morphological feature of Alzheimer disease.”
The elderly Hisayama residents of the study were examined and evaluated via MRI assessments every 6-7 years between 1985 and 2012.(11)
Brain Shrinkage Prevention
The solution for brain shrinkage in aging? You can sharply reduce your risk for brain shrinkage and Alzheimer’s disease (AD) through dietary and lifestyle interventions that counter the pathological changes in your body and brain that underly the pathology associated with brain and hippocampal shrinkage in AD and dementia.
If you are carrying around excess belly fat and you are a midlifer or older, start taking control of your risk for AD and dementia by losing the belly fat and reversing the health problems associated with it.
If you are a carrier of the ApoE4 genetic variant, excess belly and body fat and biomarkers of cardiometabolic disease are especially important and critical factors to keep a close eye on.
ApoE4 genotypes, E3/E4 and E4/E4, are linked to a higher risk for cardiovascular disease and atherosclerosis (ischemic heart disease), and ApoE4 carriers are associated with more severe brain atrophy compared with noncarriers in AD.(12,13,14)
The Solution?
Personalized nutrition, diet, and lifestyle interventions can reverse years of damage and set the foundation for a vital body and brain for the rest of your life.
My BrainDefend® Personalized Body-Brain Heath and Renewal Program is designed to take the weight off your belly and the worry of your shoulders and your mind. Structured into my BrainDefend® programs are detoxification and weight/belly fat loss programs. Contact me here to learn more and schedule your complimentary strategy session.
A final word on BMI calculations in case you are not familiar with them.
Body Mass Index and Relative Fat Mass Estimator
BMI is calculated as weight in kilograms divided by height in meters squared, rounded to one decimal place. This link will take you to an easy to use BMI calculator at: https://www.nhlbi.nih.gov/health/educational/lose_wt/BMI/bmicalc.htm
While BMI assessments are quick and easy read on a person’s weight and risk for obesity, it is not the best tool for assessing fat mass.
In certain individuals such as skinny fat types, BMI fails in the assessment of body fat mass and it’s risk for cardiometabolic disease. Sex, age, and increased muscle mass are additional confounding factors.
Additionally, in women a waist to hip ratio is generally accepted as a more precise predictor of cardiac status and risk.
BMI assessments on top athletes may also be inaccurate. Increased muscle mass translates to a higher BMI in leaner and muscular individuals with low body fat.
Bioelectrical impedance analysis (BIA) assessments may provide a more accurate assessment of body composition—fat and lean body mass—and there are many other body composition screenings such as skinfold thickness and underwater weighing that are used in clinical and sports performance settings, and are considered to be more reliable than BMI for evaluating body fat mass.
Lastly, a 2018 study revealed that Relative Fat Mass (RFM) as a new and more accurate estimator of whole-body fat percentage. Link to an RFM calculator: https://rfmcalculator.com
Endnotes
* Gray matter in the brain is the mass composed of neuronal cell bodies, capillaries, glial cells (astrocytes, microglia), dendrites, and synapses. Gray matter is the outermost layer of the brain (cerebral cortex). What’s left?
The neurons long axonal extensions are enveloped by myelin sheaths (an insulating layer) that gives the deeper mass (subcortical) in the brain its white matter color distinction.
Glial cells—astrocytes, microglia and oligodendrocytes are also present in the white matter regions of the brain. Oligodendrocytes are myelin producing glia. Note that there is an overlapping presence of astrocytes, microglia and oligodendrocytes in gray and white matter.
The axons connect all the billions of neurons (approximately 100 billion) of the brain’s gray matter which is more accurately described as being pinkish-gray due to the capillaries that supply blood to it. Once the brain expires and the blood stops flowing through the brain, that pinkish-gray matter turns to gray.
References
1. Prevalence of Obesity Among Adults and Youth: United States, 2015–2016
Craig M. Hales, M.D., Margaret D. Carroll, M.S.P.H., Cheryl D. Fryar, M.S.P.H., and Cynthia L. Ogden, Ph.D.
NCHS Data Brief, No. 288, October 2017
2. The dynamics of cortical and hippocampal atrophy in Alzheimer disease.
Sabuncu MR, Desikan RS, Sepulcre J, Yeo BT, Liu H, Schmansky NJ, Reuter M, Weiner MW, Buckner RL, Sperling RA, Fischl B,
Alzheimer’s Disease Neuroimaging Initiative.
Arch Neurol. 2011 Aug; 68(8):1040-8.
3. Very early detection of Alzheimer neuropathology and the role of brain reserve in modifying its clinical expression.
Mortimer JA, Borenstein AR, Gosche KM, Snowdon DA.
J Geriatr Psychiatry Neurol. 2005;18(4):218–223.
5. Visceral fat is associated with lower brain volume in healthy middle-aged adults.
Debette S, Beiser A, Hoffmann U, et al.
Ann Neurol. 2010;68(2):136–144.
6. Inflammatory biomarkers are associated with total brain volume: the Framingham Heart Study.
Jefferson AL, Massaro JM, Wolf PA, Seshadri S, Au R, Vasan RS, Larson MG, Meigs JB, Keaney JF Jr, Lipinska I, Kathiresan S, Benjamin EJ, DeCarli C
Neurology. 2007 Mar 27; 68(13):1032-8.
7. Hippocampal volume is related to body mass index in Alzheimer’s disease.
Ho AJ, Raji CA, Saharan P, et al.
Neuroreport. 2011 Jan;22(1):10-14.
8. Adverse Associations between Visceral Adiposity, Brain Structure, and Cognitive Performance in Healthy Elderly.
Isaac V, Sim S, Zheng H, Zagorodnov V, Tai ES, Chee M.
Front Aging Neurosci. 2011;3:12. Published 2011 Sep 13.
9. Sarcopenia in older adults.
Walston JD.
Curr Opin Rheumatol. 2012;24(6):623–627.
10. Sarcopenic obesity and cognitive performance.
Magdalena Tolea, Stephanie Chrisphonte, James Galvin.
Clinical Interventions in Aging, 2018; Volume 13: 1111
11. Association Between Diabetes and Hippocampal Atrophy in Elderly Japanese: The Hisayama Study
Naoki Hirabayashi, Jun Hata1,, Tomoyuki Ohara1, Naoko Mukai, Masaharu Nagata1, Mao Shibata1, Seiji Gotoh1, Yoshihiko Furuta1, Fumio Yamashita, Kazufumi Yoshihara, Takanari Kitazono, Nobuyuki Sudo, Yutaka Kiyohara1, and Toshiharu Ninomiya
Diabetes Care 2016 Sep; 39(9): 1543-1549
12. Apolipoprotein E ε4 is associated with disease-specific effects on brain atrophy in Alzheimer’s disease and frontotemporal dementia
Federica Agosta, Keith A. Vossel, Bruce L. Miller, Raffaella Migliaccio, Stephen J. Bonasera, Massimo Filippi, Adam L. Boxer, Anna Karydas, Katherine L. Possin, Maria Luisa Gorno-Tempini
Proceedings of the National Academy of Sciences Feb 2009, 106 (6) 2018-2022
13. Apolipoprotein E Gene Variants and Risk of Coronary Heart Disease: A Meta-Analysis.
Xu M, Zhao J, Zhang Y, et al.
Biomed Res Int. 2016:3912175.
14. Apolipoprotein E Polymorphism and Cardiovascular Disease: A HuGE Review
June E. Eichner, S. Terence Dunn, Ghazala Perveen, David M. Thompson, Kenneth E. Stewart, Berrit C. Stroehla,
American Journal of Epidemiology, Volume 155, Issue 6, 15 March 2002, Pages 487–495.