In a recently published study—NutriNet-Santé (10/2018)—that included the analysis of dietary records of 84,158 French adults that spanned between May 2009 and June 20017— the study authors concluded found that “Higher intakes of polyphenols, especially anthocyanins and catechins (flavan-3-ols), were associated with a statistically significant decreased cardiovascular disease risk.”(1).
The polyphenol intake was primarily derived from coffee (49%), tea (23%), fruits (17%), vegetables (8%), and wine (5%).
Polyphenols
The polyphenol family—powerful anti-inflammatory and antioxidant modulating compounds found in foods and beverages, comprise two subclasses that are generally grouped into flavonoids and non-flavonoids.
Flavonoids compose the largest class of commonly consumed polyphenols and include the flavonoid subclasses: flavonols, flavan-3-ols, flavones, flavanones, isoflavones and anthocyanins.
Three major non-flavonoid groups include phenolic acids found in berries and tea, stilbenes (e.g, trans-resveratrol found in grapes and wine), and lignans that found in fruits, vegetables, legumes, grains and in many seeds such as flaxseed.
 While the NutriNet-Santé study focused on the cardiovascular benefits of polyphenols, similar studies (PREDIMED study),that include the dietary patterns ascribed to the Mediterranean diet that is naturally rich in polyphenols have shown a protective and vitalizing effect on cognitive function that contribute to memory and learning processes.(2)
While the NutriNet-Santé study focused on the cardiovascular benefits of polyphenols, similar studies (PREDIMED study),that include the dietary patterns ascribed to the Mediterranean diet that is naturally rich in polyphenols have shown a protective and vitalizing effect on cognitive function that contribute to memory and learning processes.(2)
This is of particular importance in halting the cognitive impairment that is typical of age-related diseases such as type 2 diabetes, cardiovascular disease and late-onset Alzheimer’s disease.
What is bad for the heart is bad for the brain
“The heart-brain connection”, is now proposed as an important awareness for mitigating the risk for dementia. However, while the term has been popularized of late, the link of cardiovascular disease to dementia has been recognized for many years.
Unfortunately, there is a lack of patient education from physicians to their patients about the risk of dementia that may result from chronic cardiovascular disease, and a concurrent absence of awareness by many clinicians about how vital early intervention and assessment is in reducing the risk for dementia.
The term cardiovascular, describes your heart (cardio) and vascular system, and the integrity of the latter is critical to the health of your heart and brain.
If you have an advanced vascular disease process, such as coronary artery disease that is often caused by atherosclerosis, the buildup of plaque and the reduced circulation that comes from narrowing of the arteries inhibits the delivery of oxygen (ischemia) and nutrients, and puts a strain on your heart and your brain.
A finding from the Rotterdam study* that began in 1990 and collected data up to 2008 in approximately 15,000 individuals 45 years of age and older, determined that atherosclerosis was associated with Alzheimer’s disease and vascular dementia, and that the ApoE4 gene variant’s role in atherosclerosis (narrowing of the arteries from plaque buildup) is a factor in the onset of Alzheimer’s.(3)
For more information on ApoE4, please read my article: “The Alzheimer’s Gene Puzzle—The ApoE4 Variant As A Risk Factor”.
The term “cardiogenic dementia” first surfaced an editorial published in the prestigious Lancet Journal in 1977.(4) Since then, the understanding of how cardiovascular disease can substantially increase the risk for vascular dementia has been well studied.
The strain on your heart over time that is derived from impaired vascular circulation results in a risk for a host of cardiovascular complications that include hypertension, heart failure, angina, and peripheral artery disease.
Peripheral artery disease, also termed peripheral vascular disease, refers to the narrowing of the peripheral arteries in your limbs, and organs which can result in kidney disease.
Peripheral artery disease and the reduction of blood flow to the brain (Cerebral Hypoperfusion), not only puts you at risk for stroke, it is strongly associated with the increased risk for vascular dementia and Alzheimer’s disease.(5)
Abnormal heart rhythm—cardiac arrhythmias, also pose a risk for stroke, cognitive decline and dementia.(6)
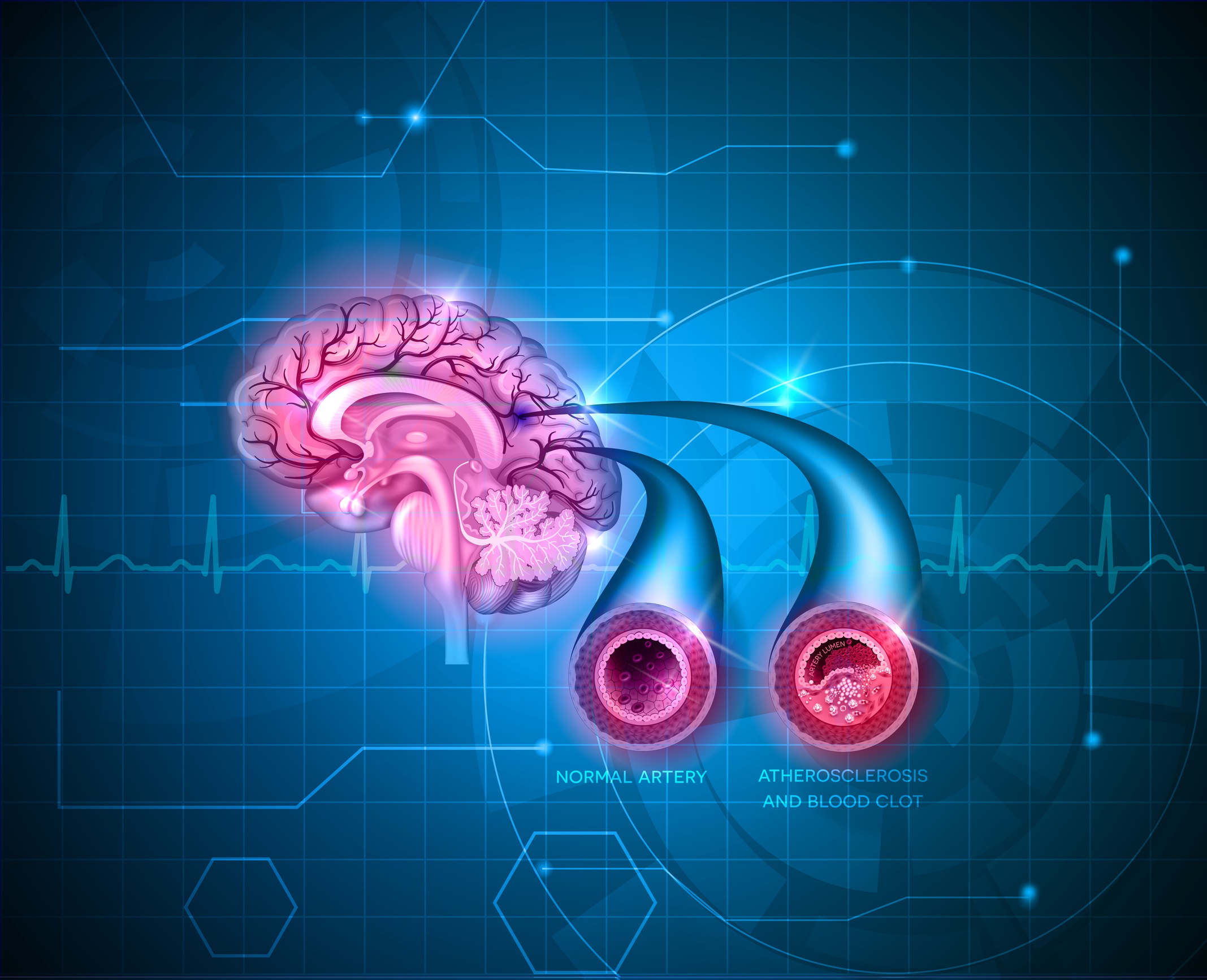
Normal cerebral artery and artery with atherosclerosis and blood clot. The second artery to the right of the illustration with the blood clot depicts the impeded blood flow.
Reducing the risk for dementia
Once the vascular disease process extends to a circulatory disease process that affects the brain’s microcirculation, it is termed cerebrovascular disease. “One in three of us will have a stroke, become demented, or both.”(7)
The lack of an all too common clinical recognition that prompts a proactive approach to prevention is certainly not due to the lack of research and evidence that links the complications of cardiovascular disease to dementia.
Case in point is the National Institute of Neurological Disorders and Stroke (NINDS)—an “Institute within the National Institutes of Health that aims to seek fundamental knowledge about the brain and nervous system and to use that knowledge to reduce the burden of neurological disease.”
NINDS is committed to reducing stroke and the incidence of neurological disease through biomedical research. Please visit their page Brain Basics: Preventing Stroke @
https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Preventing-Stroke
Polyphenols derived from diet and supplementation not only reduce the risk for cardiovascular disease (CVD), they enhance vascular function and flow, and provide powerful protection against the development and progression of more advanced complications of cardiovascular and cerebrovascular disease (cerebro-cardiovascular disease) that include stroke, vascular dementia, and late-onset Alzheimer’s disease.(8)
Chronic inflammation and oxidative stress are principle mechanisms that are inherent pathological mechanisms in the progression of cerebro-cardiovascular disease.
Thus, anti-inflammatory and antioxidant therapies and protocols centered on nutrition are imperative interventions for mitigating the risk of these disease pattens and the onset of vascular dementia and Alzheimer’s disease.
Dietary patterns such as a low-carb Mediterranean diet, and “The Mind Diet” that I expand on in The Improved Mind Diet are crucial nutrition road maps for optimizing health and reducing the incidence of these age-related disorders.
For more information on how diet and polyphenols protect against the onset of Alzheimer’s disease as you age, please read: “Blueberry Polyphenols Protect the Brain from the Degenerative Processes Associated with Brain Aging and Alzheimer’s Disease”
My second book, The Improved Mind Diet, provides a comprehensive overview on how polyphenols and other dietary factors optimize cognitive function and protect against CVD, type 2 diabetes and late-onset Alzheimer’s disease.
Please get on the list to be notified about its availability.
Endnotes
* The primary objectives of the Rotterdam Study were to investigate the risk factors of cardiovascular, neurological, psychiatric, ophthalmological and endocrine diseases in the elderly.
“Participants were followed for the most common diseases in the elderly, including coronary heart disease, heart failure and stroke, Parkinson’s disease, Alzheimer’s disease and other dementias, depression and anxiety disorders, macular degeneration and glaucoma, diabetes mellitus and osteoporosis.”
The findings of the study have been presented in over 1500 research articles and reports.
Rotterdam Study website: http://www.erasmus-epidemiology.nl/research/ergo.htm
References
1. Prospective Association between Total and Specific Dietary Polyphenol Intakes and Cardiovascular Disease Risk in the Nutrinet-Santé French Cohort
Adriouch, S.; Lampuré, A.; Nechba, A.; Baudry, J.; Assmann, K.; Kesse-Guyot, E.; Hercberg, S.; Scalbert, A.; Touvier, M.; Fezeu, L.K.
Nutrients 2018, 10(11), 1587
2. Mediterranean Diet and Age-Related Cognitive Decline: A Randomized Clinical Trial.
Valls-Pedret C, Sala-Vila A, Serra-Mir M, et al.
JAMA Intern Med. 2015;175(7):1094–1103
3. Atherosclerosis, apolipoprotein E, and prevalence of dementia and Alzheimer’s disease in the Rotterdam Study.
Hofman A, Ott A, Breteler MM, Bots ML, Slooter AJ, van Harskamp F, van Duijn CN, Van Broeckhoven C, Grobbee DE.
Lancet. 1997 Jan 18;349(9046):151-4.
4. Heart failure and cognitive impairment: challenges and opportunities
Heckman GA, Patterson CJ, Demers C, St Onge J, Turpie ID, McKelvie RS.
Clin Interv Aging. 2007;2(2):209-18.
5. “Cardiovascular Risk Factors Promote Brain Hypoperfusion Leading to Cognitive Decline and Dementia,”
Jack C. de la Torre
Cardiovascular Psychiatry and Neurology, vol. 2012, Article ID 367516, 15 pages, 2012.
6. Atrial Fibrillation, Cognitive Decline And Dementia.
Alonso A, Arenas de Larriva AP.
Eur Cardiol. 2016;11(1):49-53.
7. Stroke and Vascular Cognitive Impairment
A Transdisciplinary, Translational and Transactional Approach
Vladimir Hachinski
The 2005 Thomas Willis Lecture
8. Polyphenols and Microvascular Function in Humans: A Systematic Review
Kirsty Roberts, Richard Draijer, Dick H J Thijssen, David Low
Current Pharmaceutical Design. 2018/04/01 Vol.24(2):203-226